Spotting Amyloidosis Early: Common Warning Signs
Understanding Amyloidosis: An Overview
Amyloidosis is a complex condition characterized by the accumulation of amyloid proteins in various tissues and organs. These proteins are abnormal and can lead to significant health complications if not identified and managed early. The importance of understanding amyloidosis lies in its potential to affect multiple body systems, making early detection critical. This condition is not a single disease but a group of diseases, each with its specific protein type and deposition pattern. Recognizing the signs and symptoms can significantly impact the management and outcomes for those affected.
The condition can be classified into several types, including primary amyloidosis, secondary amyloidosis, and hereditary amyloidosis. Each type has distinct causes and implications for health. Primary amyloidosis, for instance, is often related to plasma cell disorders, while secondary amyloidosis is associated with chronic inflammatory conditions. Hereditary amyloidosis is linked to genetic mutations that cause abnormal protein production. Understanding these distinctions is essential for effective diagnosis and treatment.
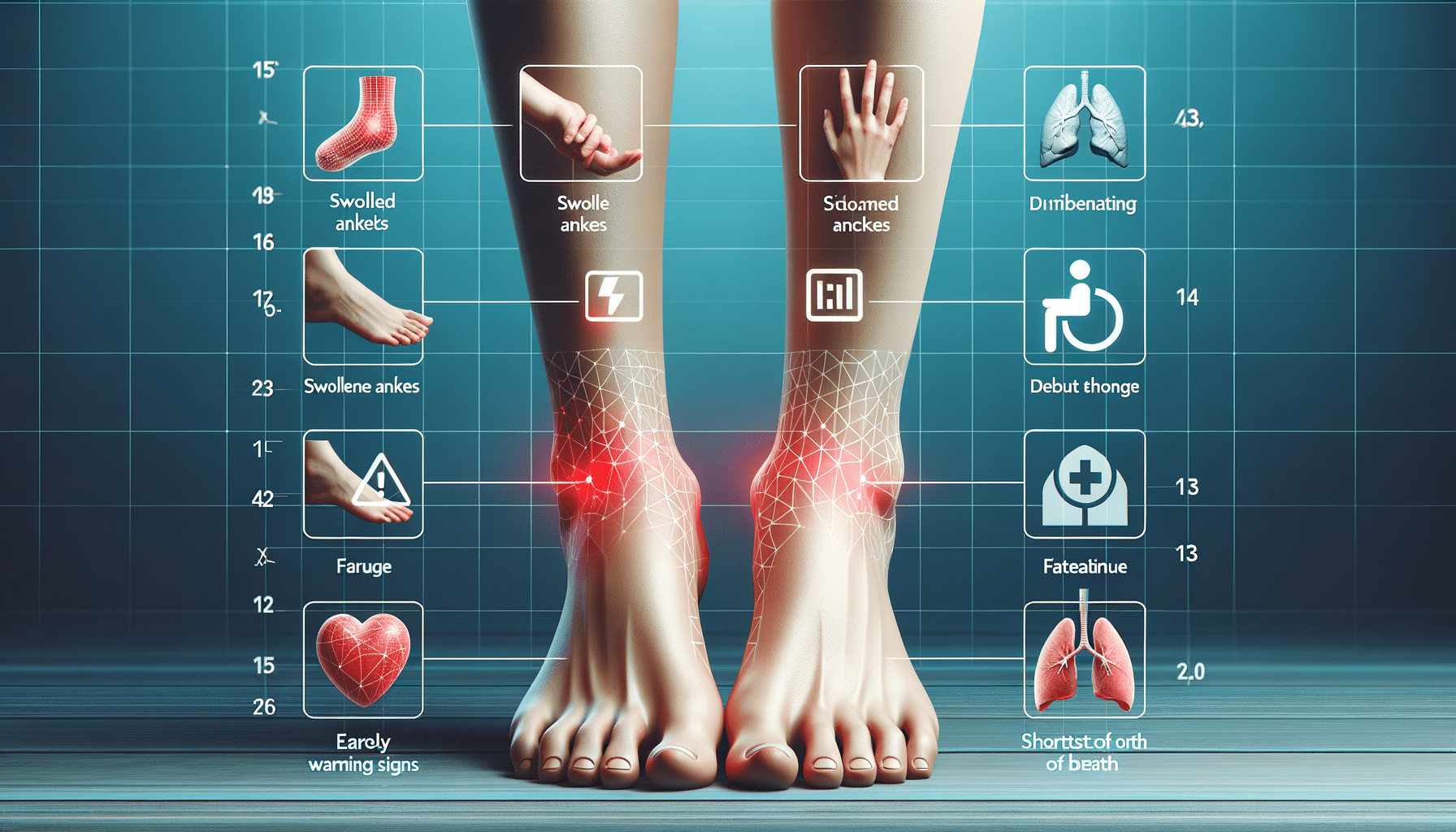
Key to managing amyloidosis is early detection, which can be challenging due to the nonspecific nature of its symptoms. Common signs include fatigue, weight loss, and swelling in various body parts. However, these symptoms can easily be mistaken for other conditions, underscoring the need for increased awareness and education about amyloidosis. By recognizing the early warning signs, individuals can seek timely medical advice and potentially improve their prognosis.
Symptoms and Diagnosis of Amyloidosis
Amyloidosis presents a wide range of symptoms depending on the organs affected by amyloid deposits. This variability can complicate diagnosis, as the symptoms often mimic those of other diseases. Common symptoms include unexplained weight loss, severe fatigue, and swelling in the ankles and legs. Patients may also experience numbness or tingling in the hands and feet, known as peripheral neuropathy, which can significantly impact daily life.
Diagnosing amyloidosis typically involves a combination of clinical evaluation and laboratory tests. A biopsy is often necessary to confirm the presence of amyloid deposits in tissues. This procedure involves extracting a small tissue sample from an affected organ, such as the kidney, liver, or heart, and examining it under a microscope. Blood and urine tests can also help identify abnormal protein levels, providing further clues to the diagnosis.
Advanced imaging techniques, like echocardiograms and MRI scans, can assess the extent of organ involvement and guide treatment decisions. These tools are invaluable for visualizing the impact of amyloid deposits on organ function, particularly in the heart and kidneys. Early and accurate diagnosis is crucial for managing amyloidosis effectively, as it allows healthcare professionals to tailor treatment strategies to the specific needs of each patient.
Treatment Options for Amyloidosis
Treating amyloidosis involves addressing the underlying cause of amyloid protein production and managing symptoms to improve quality of life. The treatment approach varies depending on the type of amyloidosis and the organs affected. For primary amyloidosis, therapies often focus on reducing the production of amyloid proteins. This may involve chemotherapy drugs used in treating related plasma cell disorders, as they can help decrease the number of abnormal cells producing amyloid proteins.
In cases of secondary amyloidosis, managing the underlying inflammatory condition is key. This might involve using medications to control inflammation and reduce the production of amyloid proteins. For hereditary amyloidosis, treatment options may include liver transplantation, particularly when the liver is the primary site of amyloid production. This approach can be effective in halting the progression of the disease, especially in familial types where specific proteins are produced in the liver.
Supportive care is also an essential component of treatment, focusing on alleviating symptoms and maintaining organ function. This can include medications to manage heart failure symptoms, diuretics to reduce swelling, and dietary modifications to support kidney function. Emerging therapies, such as targeted drugs and gene therapy, are being explored to provide more effective treatment options for amyloidosis patients.
The Impact of Amyloidosis on Daily Life
Living with amyloidosis can be challenging, as the condition often affects multiple aspects of daily life. The symptoms, such as fatigue and neuropathy, can significantly impact an individual’s ability to perform everyday tasks. This can lead to a reduced quality of life and increased reliance on others for support. Understanding these challenges is crucial for providing comprehensive care and support to individuals affected by amyloidosis.
Many patients experience emotional and psychological effects due to the chronic nature of the disease and its impact on their lifestyle. Coping with a long-term condition requires resilience and adaptability, and patients often benefit from psychological support and counseling. Support groups and community resources can also provide valuable assistance, offering a platform for sharing experiences and coping strategies.
Managing amyloidosis requires a multidisciplinary approach, involving healthcare professionals from various fields. Regular monitoring and follow-up care are essential to manage symptoms and prevent complications. Patients are encouraged to maintain open communication with their healthcare team and actively participate in their treatment plans. This collaborative approach can enhance the overall management of amyloidosis, improving outcomes and quality of life for those affected.
Future Directions in Amyloidosis Research and Treatment
The field of amyloidosis research is rapidly evolving, with ongoing studies aimed at improving diagnosis and treatment options. Advances in genetic research are shedding light on the hereditary forms of the disease, offering hope for more targeted therapies. Understanding the genetic mutations involved in amyloid protein production can lead to the development of drugs that specifically target these pathways, potentially reducing the burden of the disease.
Innovative treatment approaches, such as monoclonal antibodies and small molecule inhibitors, are being explored to disrupt amyloid fibril formation. These therapies hold promise in altering the disease course and improving patient outcomes. Clinical trials are underway to evaluate the efficacy and safety of these novel treatments, providing hope for more effective management strategies in the future.
In addition to therapeutic advancements, efforts are being made to enhance early detection and diagnosis of amyloidosis. Biomarker research is a promising area, with the potential to identify specific proteins or genetic markers associated with the disease. This could lead to the development of non-invasive diagnostic tests, enabling earlier intervention and improved prognosis for patients. As research progresses, the future of amyloidosis treatment looks increasingly hopeful, with the potential for significant improvements in patient care and outcomes.