What is Amyloidosis?
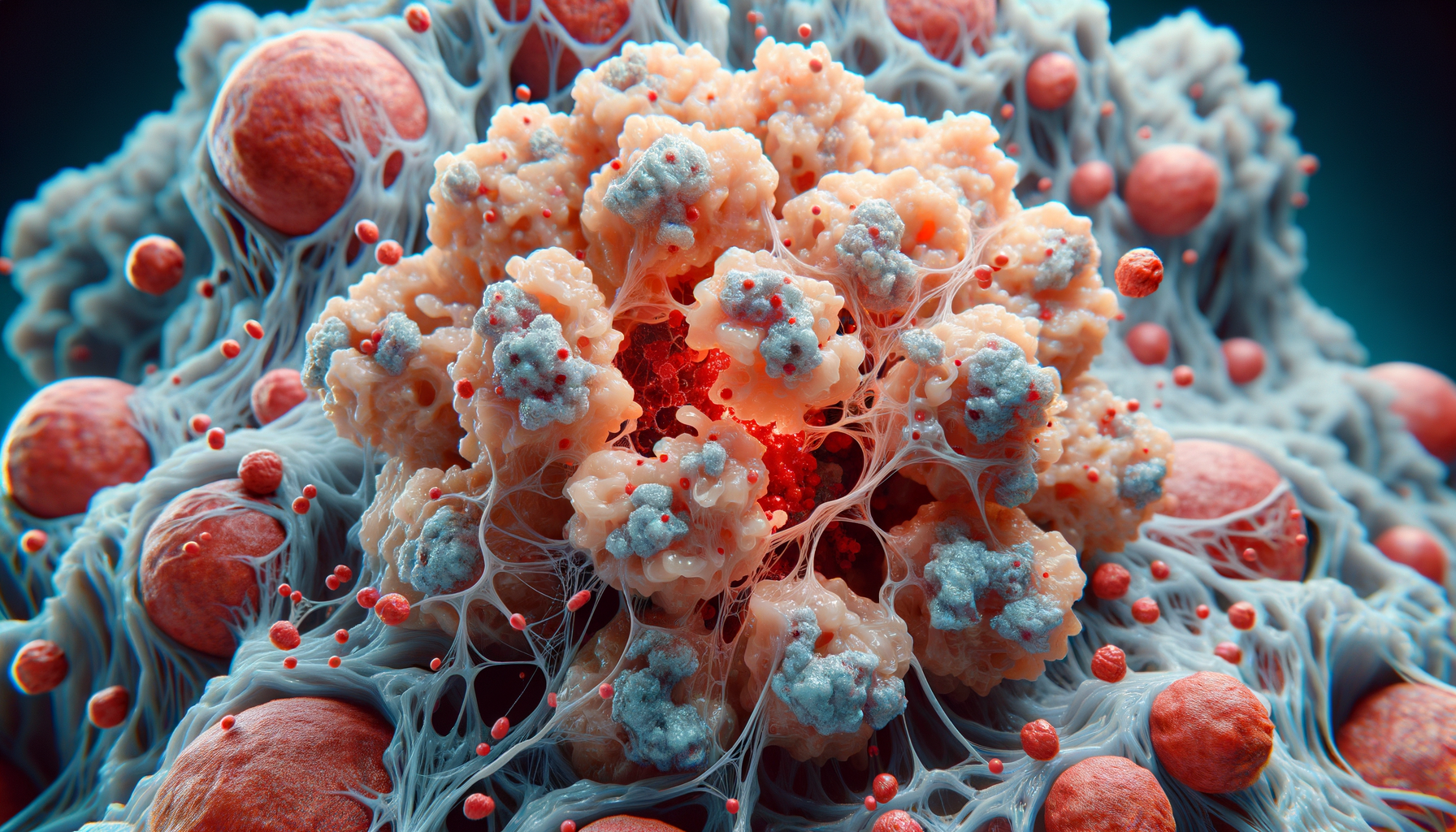
Amyloidosis is a rare but serious condition characterized by the abnormal deposition of amyloid proteins in various tissues and organs. These proteins can accumulate in different parts of the body, leading to a range of symptoms and complications depending on the organs affected. Amyloid proteins are misfolded proteins that the body cannot break down, causing them to build up and interfere with normal bodily functions. The condition can be systemic, affecting multiple organs, or localized to one specific area.
There are several types of amyloidosis, each defined by the specific protein involved. The most common types include AL (light chain) amyloidosis, AA (secondary) amyloidosis, and hereditary or familial amyloidosis. AL amyloidosis, the most prevalent form, results from an abnormality in plasma cells, which produce antibodies. AA amyloidosis often occurs in response to chronic inflammatory diseases, while hereditary amyloidosis is caused by genetic mutations passed down through families.
The complexity of amyloidosis arises from its diverse manifestations and the difficulty in diagnosing it early. Symptoms can vary widely, from fatigue and weight loss to more severe organ dysfunction. As such, understanding the type and extent of amyloid buildup is crucial for effective management and treatment.
Symptoms and Diagnosis
The symptoms of amyloidosis are as varied as the condition itself, often depending on which organs are affected. Common symptoms include fatigue, unexplained weight loss, swelling in the legs or ankles, numbness or tingling in the hands and feet, and shortness of breath. More severe symptoms might involve heart failure, kidney dysfunction, or gastrointestinal issues.
Diagnosing amyloidosis can be challenging due to its non-specific symptoms that overlap with many other conditions. Healthcare professionals typically begin with a thorough medical history and physical examination, followed by laboratory tests to detect amyloid proteins in the blood or urine. Imaging studies, such as echocardiograms or MRIs, may be used to assess organ involvement.
A definitive diagnosis often requires a tissue biopsy, where a small sample of affected tissue is examined for amyloid deposits. This biopsy can be taken from different areas, including the abdominal fat pad, bone marrow, or directly from the affected organ. Once amyloidosis is confirmed, further tests are conducted to determine the specific type, which is essential for guiding treatment decisions.
Treatment Options
Treatment for amyloidosis depends on the type and extent of the condition, as well as the organs involved. The primary goal is to reduce the production of amyloid proteins and manage symptoms to improve quality of life. For AL amyloidosis, treatment often involves chemotherapy to target the abnormal plasma cells producing the amyloid light chains. This approach is similar to treatments used for multiple myeloma.
In cases of AA amyloidosis, addressing the underlying inflammatory condition is crucial. This may involve the use of anti-inflammatory medications or biologics to control diseases like rheumatoid arthritis or chronic infections. For hereditary amyloidosis, liver transplantation might be considered, as the liver produces the amyloidogenic protein in many hereditary cases.
Supportive care is also an integral part of managing amyloidosis. This can include medications to manage symptoms such as heart failure or kidney dysfunction, dietary modifications, and lifestyle changes. In recent years, new therapies targeting amyloid deposits directly have been developed, offering hope for improved outcomes.
Living with Amyloidosis
Living with amyloidosis can be challenging, given the chronic nature of the condition and its impact on daily life. Patients often require ongoing medical care and monitoring to manage symptoms and prevent complications. It is essential for individuals with amyloidosis to work closely with a healthcare team familiar with the condition, including specialists such as hematologists, cardiologists, and nephrologists.
Emotional and psychological support is equally important, as dealing with a chronic illness can be emotionally taxing. Support groups and counseling can provide valuable resources and a sense of community for patients and their families. Education about the condition and staying informed about new treatments and research can empower patients to take an active role in their care.
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate rest, can help manage symptoms and improve overall well-being. Patients are encouraged to communicate openly with their healthcare providers about any changes in symptoms or concerns they may have.
Research and Future Directions
Research into amyloidosis is ongoing, with scientists and clinicians striving to better understand the condition and develop more effective treatments. Advances in genetic research have shed light on the hereditary forms of amyloidosis, leading to improved genetic testing and counseling for affected families.
New therapeutic approaches are being explored, including drugs that stabilize amyloidogenic proteins, preventing them from misfolding and forming deposits. Additionally, clinical trials are investigating the use of monoclonal antibodies to target and clear existing amyloid deposits from the body.
The future of amyloidosis treatment looks promising, with ongoing research focusing on early detection and personalized medicine approaches. As our understanding of the condition grows, so does the potential for innovative therapies that could significantly improve outcomes for patients living with amyloidosis.



Leave a Reply